Chronic underinvestment in the public health system has resulted in severe workforce shortages across health sector occupations and a substantial gap in addressing unmet health needs.
Funding increases to value, support and train the workforce are vital both for those working in the health system and those using it.
“If we are serious about rebuilding the health system that works for us all, we need to frontload resourcing and power it up. Budget 2023 suggests the Government lacks a real commitment to meet this goal”.
Sarah Dalton, Executive Director, ASMS
STATE OF THE SECTOR
Aotearoa New Zealand’s public health system has failed to meet health needs over many years due to chronic under-investment. This effect has been felt particularly for marginalised groups, including Māori, Pasifika, and tāngata whaikaha. Significant funding increases are needed to value, support, and train the workforce and deliver essential reforms. Poor health outcomes have increased with user-charges in primary care, creating barriers to those most in need of health services.
Our total (public and private) health expenditure, measured as a proportion of GDP, has remained well below other comparable countries for decades.
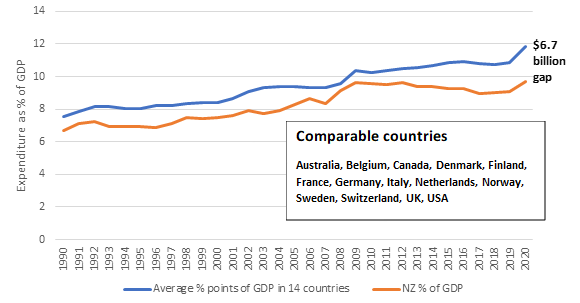
Globally, government responses to the Covid-19 pandemic drove spending upwards in 2020. In terms of expenditure as a percentage of GDP, Aotearoa New Zealand needed to have invested an additional $6.7 billion in 2020 to equal the average of the 14 comparable countries.
The health workforce accounts for about two-thirds of health investment. The funding shortfall led to a long-standing workforce shortage across health sector occupations. Our health and social workforce needs 60,000 new workers to match the average workforce capacity of comparable countries.
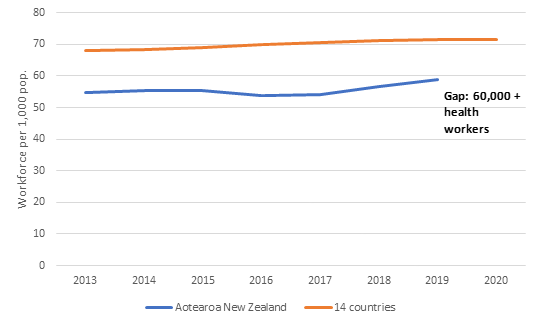
We are not training or retaining enough staff, and barriers include poor working conditions, inadequate pay, gender discrimination and heavy workloads.
Last year’s health infrastructure budget of $1.3 billion over two years focused on the most urgent and critical needs. Decades of capital under-investment has resulted in a long list of deteriorating buildings and equipment waiting to be fixed with estimated costs of between $14 billion and $22 billion.
Budget 2023
Budget 2023 marks the second year of the move to multi-year health funding and the establishment of heath entities Te Whatu Ora and Te Aka Whai Ora.
The 2023 Budget headlines for health include:
- Removing the $5 prescription co-payment for all New Zealanders at a cost of $618.6 million over four years
- A nearly $400 million investment in the delivery of Hauora Māori services
- $20 million to establish outreach services to lift immunisation and screening and implement initiatives that increase life expectancy of Māori and Pacific peoples
- $125 million increase to PHARMAC’s budget for pharmaceuticals purchasing, which will likely maintain the current availability of pharmaceuticals
- $63 million to deliver safe staffing initiatives and 500 new nurses
- $2.2 billion to resolve historical non-compliance with the Holidays Act 2003
- $3.1 billion for capital investment, largely for infrastructure projects is welcome in a sector needing up to an estimated $22 billion
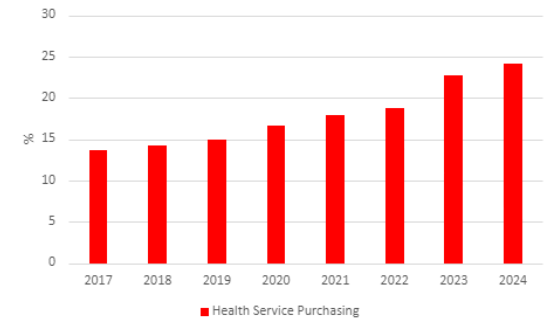
If we exclude the funding made available as a consequence of COVID-19, the purchasing of health services overall has increased significantly since 2017, from $13.6 billion to a forecast $24.1 billion in 2024.
WHAT DO WE THINK OF THE BUDGET ACTIONS?
There was an opportunity in Budget 2023 to commit additional funding beyond the $1.3 billion uplift already announced in Budget 2022. In the context of limited spending in Budget 2023, some important initiatives address cost-of-living issues that can restrict patient and whānau access to primary and community care.
Any increases to workforce numbers and pay are welcome, but more work must be done to make sure that we have the health workforce and resources we need.
WILL THE INITIATIVES SOLVE THE KEY PROBLEMS OF THE SECTOR?
Budget 2023 maintains the recent trend in increases in expenditure. Aotearoa New Zealand requires sustained investment in health to meet its challenges.
Hospital and specialist services have increased by a preliminary estimate of four per cent. This increase is a cut in real terms when adjusted from forecast inflation and demographic pressures. Funding for primary, community, public and population health services, receives a 2.4 per cent increase, another cut in real terms.
We applaud the removal of prescription co-payments. However, GP or Nurse Practitioner appointment is still required to receive a prescription. Three per cent of New Zealanders report prescription costs as a barrier to care; yet in 2021, 27.9 per cent of adults experienced one or more barriers to primary health care. In 2022, 10.7 per cent of adults were unable to access a GP due to cost.
WHAT’S MISSING?
Workforce shortages are the biggest issue for the health sector. While 500 nurses are a welcome start, this is an estimated ten per cent of the current nursing workforce shortage.
The initiatives described in the Budget will not be enough to relieve all the pressures on the health system. It will be interesting to examine how the $118 million to reduce waiting lists by freeing up hospital beds works. Is it more private provision? In which case it may stretch the workforce further across the private and public sectors.
WHAT SHOULD THE LONGER-TERM STRATEGY BE?
The goal must be good health for all: improving the health of the whole population while also improving health equity. This requires coordinated, cross-government action to address determinants of ill health and increase the capacity of community and hospital services. Substantial further investment is needed to address the health and disability workforce crisis. This includes improvements in education, training, recruitment and retention, along with developing workforce equity and diversity. These improvements must be guided by a comprehensive workforce plan supported by the necessary investment.
Although scrapping $5 prescription co-payments is a positive step towards enabling access to medicines, many struggle financially to access primary care services in the first place due to user-charges. A fully-free public healthcare system must be the vision for our reformed healthcare sector.